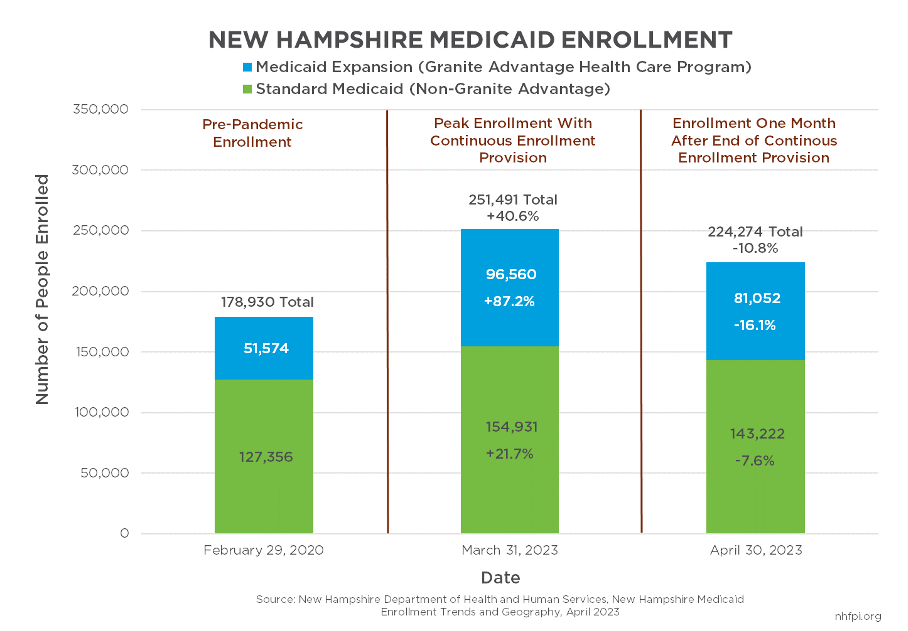
At the onset of the COVID-19 pandemic, the federal government implemented a policy to provide additional Medicaid funds to states and restricted the ability of states to disenroll people from Medicaid, requiring continuous enrollment. The number of Granite Staters accessing health coverage through Medicaid increased 40.6 percent during this period, with Medicaid Expansion program enrollment for adults with low incomes rising 87.2 percent. The federal continuous enrollment provision expired on April 1, 2023, and New Hampshire began disenrolling people from Medicaid based on their eligibility using pre-pandemic rules. At the end of April 2023, total Medicaid enrollment had declined by 27,217 people (10.8 percent) relative to the end of March 2023, led by a 15,508 (16.1 percent) decline in the Medicaid Expansion population. Total enrollment remained 45,344 (25.3 percent) higher than it was immediately before the pandemic reached New Hampshire.
The State plans to continue phased Medicaid disenrollments resulting from the end of the continuous enrollment provisions over the next twelve months. New Hampshire is one of five states nationally that began disenrollments for procedural reasons in the first month following the end of the federal continuous enrollment provision.