In response to the COVID-19 pandemic, the federal government and state governments enhanced access to health coverage by permitting people to stay on Medicaid continuously after their initial qualification and enrollment. The continuous enrollment provision allowed millions of U.S. residents who lost employment to retain health coverage as they rebuilt their household incomes without verifying their continued eligibility during a public health crisis. This federal Medicaid policy ended on March 31, 2023, and April 1, 2024 marked one year since New Hampshire began disenrolling Medicaid recipients after this provision expired. Since the end of this policy, total Medicaid enrollment across the state has declined by 26.7 percent, with notable differences among children, working-age adults with low incomes, and individuals experiencing disabilities. Despite this sharp decline, total Medicaid enrollment remains higher than before the pandemic.
Federal Guidance Surrounding the Continuous Enrollment Provision
As part of the March 2020 federal Families First Coronavirus Response Act, states were temporarily required to keep Medicaid beneficiaries continuously enrolled in coverage throughout the Public Health Emergency (PHE) in exchange for additional federal funding for their state Medicaid programs. The COVID-19-related PHE was declared in January 2020. In typical Medicaid operations, New Hampshire requires enrollees to renew their benefits annually with occasional earlier redeterminations if there are changes in circumstances, such as changes in income. The continuous enrollment provision was in effect from March 18, 2020 until shortly after the passage of the 2023 Consolidated Appropriations Act, which required the continuous enrollment provision to expire prior to the conclusion of the PHE. As a result, on April 1, 2023, states had the option to begin disenrolling beneficiaries from Medicaid through a process known as the unwind.
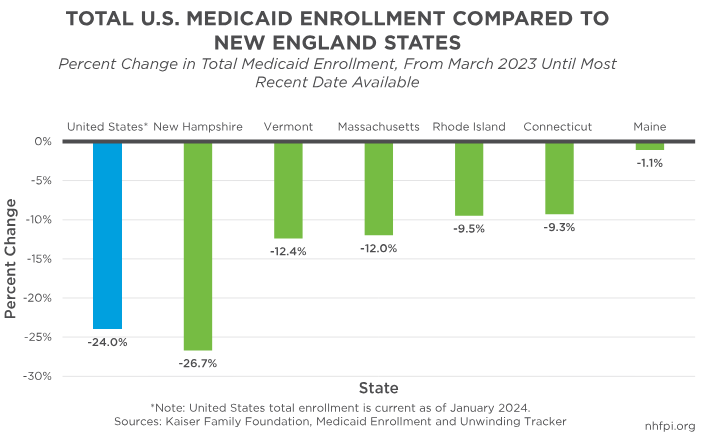
As of April 11, 2024, approximately 31 percent of Medicaid beneficiaries nationwide who have completed the renewal process have been disenrolled from coverage, according to the Kaiser Family Foundation (KFF). Of all March 2023 enrollees, about 31 percent did not have renewal paperwork processed, as unwind policies and timing have been different across the states. For example, Maine did not begin renewals and potential disenrollments until substantially later than New Hampshire, and paused procedural disenrollments entirely until July 2024. Disenrollment rates for people who have had renewal processes completed vary from 56 percent in Utah to 12 percent in Maine, with New Hampshire’s 36 percent rate higher than 35 of the 50 states. KFF analysis also shows that, comparing total Medicaid enrollment changes from March 2023 to the most recent data available as of mid-April 2024, New Hampshire had the sixth-highest cumulative percentage decrease in enrollment, with a 26.7 percent decline. This percentage decrease is substantially larger than the neighboring states of Vermont (-12.4 percent), Massachusetts (-12.0 percent), and Maine (-1.1 percent), the last of which has paused key disenrollments following a much later initial start than New Hampshire. States beginning their disenrollment processes at varying times likely explains some of the differences among state disenrollment levels. New Hampshire reported a much higher renewal rate for those due for renewal in December 2023 data than Maine, and the highest rate among the New England states, indicating it is likely closer to completing the unwinding process than its neighbors.
Although data characterizing child Medicaid enrollments across all fifty states are limited, KFF estimates that children have made up about 37 percent of the total number of disenrolled people in the United States. Following the sharp declines in children’s enrollment across the county, the federal Centers for Medicare and Medicaid Services (CMS) released updated guidance to states in December 2023. This guidance highlighted federal renewal requirements, urged targeted outreach for children with special health needs, and outlined additional strategies to help keep more children enrolled, such as increasing automated renewal (or ex parte) rates, suspending or eliminating premiums and administrative fees, and providing multi-annual continuous coverage.
In an effort to increase enrollee retention and reduce the administrative burden on state agencies, in June 2023, CMS provided states the option to adopt temporary exceptions to usual Medicaid rules, also known as waivers. These waivers can be used to increase assistance with renewal paperwork for enrollees (including delays in disenrollment while outreach is conducted), reinstate eligible beneficiaries who lost coverage for procedural reasons, and improve ex parte renewal rates. With ex parte practices, states utilize information made available to the agency, such as income information, to automatically retain individuals without requiring them to complete renewal paperwork. New Hampshire has adopted four waivers, three of which are designed to increase ex parte renewal rates. Use of waivers may be a key factor contributing to New Hampshire’s very significant increase in the percentage of beneficiaries who have been redetermined via ex parte, from its lowest of 18 percent in May 2023 to 78 percent in March 2024.
To help people who have lost Medicaid coverage retain access to health services, CMS gave beneficiaries the option to enroll in health plans on the federal health care marketplaces established by the 2010 Patient Protection and Affordable Care Act. Typically, potential purchasers must wait until the Open Enrollment period, which runs from November 1 until January 15 during normal operations. The federal marketplace, known as the Affordable Care Act Marketplace or the health care “exchange,” provides a venue for individuals to see and compare available private-sector health insurance options, and potentially access subsidies to purchase those plans. From March 31, 2023 until the recently extended date of November 30, 2024, eligible individuals can submit an application at any point during this period to access coverage through the marketplace.
New Hampshire’s Approach to the Unwind
New Hampshire began the unwind process relatively early, starting the first set of renewals since the pandemic reached New Hampshire in February 2023, and joining three other states in beginning disenrollment in April 2023, the earliest permissible month. In preparation for the unwind, the New Hampshire Department of Health and Human Services (DHHS) sent over 120,000 “pink notices” informing beneficiaries that they would be losing coverage and providing information on how to renew, which the DHHS reported improved renewal rates by an estimated 30 percent. Additional outreach was conducted via phone to 40,000 enrollees, targeting households with children, individuals experiencing disabilities, older adults, and other prioritized groups. The DHHS also sent subsequent “yellow notices” when it was time to renew, and later “blue notices” indicating an individual had passed their coverage redetermination date but has 90 days to renew without a break in coverage.
New Hampshire’s unwind process began by prioritizing disenrollment of a “protected” group who would have lost Medicaid coverage if not for the continuous enrollment provision. Beneficiaries in the protected group included those who had exceeded Medicaid’s income limits or became categorically ineligible (such as children who aged out) during the PHE, those who did not recently engage with the health system or their Medicaid benefits, and those who were delayed in completing their last renewal and were likely to become ineligible as continuous enrollment expired. Following the unwind of the protected group, the remaining groups in the unwind sequence followed a specific order: “Granite Advantage” adult-only households, children, individuals with disabilities, those in nursing homes, and enrollees receiving Home and Community Based Services (HCBS). “Granite Advantage” refers to the New Hampshire Granite Advantage Health Care Program, which is the state’s implementation of the part of Medicaid expanded by the federal Patient Protection and Affordable Care Act to provide coverage to adults with incomes below 138 percent of the Federal Poverty Guidelines, or about $35,632 for a family of three in 2024.
According to the DHHS, as of March 2024, 67,351 Medicaid beneficiaries (34.5 percent of all Medicaid beneficiaries with enrollment renewals due in the last twelve months) lost coverage at some point throughout the unwind process. For the 28 percent of individuals who lost coverage due to their incomes being over eligibility limits, the DHHS made 24,472 referrals to the marketplace to connect people with private insurance options. Including the total number of disenrollments among both the protected and unprotected groups, about 48 percent of disenrollments were due to beneficiaries not renewing their coverage. Common reasons for choosing not to renew could include obtaining other insurance, moving out of state, changes in health conditions, or mortality. According to data provided by the DHHS, between March 2023 and April 2024, 9,645 individuals did not renew their coverage because they either passed away, moved out of state, or indicated that they did not want Medicaid coverage anymore. In addition, the percentage of those not renewing their coverage also encompasses otherwise eligible individuals who did not renew before procedural disenrollment by the DHHS. This percentage includes a key group who may not have been fully informed of their anticipated coverage loss despite DHHS efforts, such as those who changed their contact information and were unreachable, as well as those who did not complete necessary requirements and paperwork before their disenrollment deadline. According to preliminary CMS data, of the 184,955 Granite Staters who were up for renewal between March 2023 and February 2024, 51,503 (27.8 percent) had their coverage terminated for procedural reasons.
Despite the high disenrollment percentages, many eligible beneficiaries have regained coverage following their procedural disenrollment. The current Medicaid redetermination period of 90 days after disenrollment allows beneficiaries to complete the necessary requirements to renew their coverage if they are still eligible; beneficiaries temporarily retain coverage during this period. According to the DHHS, slightly more than half of renewals are processed within 30 days of the redetermination period for the protected population. Among the protected population who lost coverage, 11,139 (10.7 percent) had regained coverage as of April 1, 2024. The percent of protected children who regained coverage was higher, at 16.4 percent. Procedural disenrollments for those still eligible, however, may leave many Granite Staters without insurance coverage if they do not complete the necessary renewal requirements on time.
Decreases in Overall Medicaid Enrollment Across the State
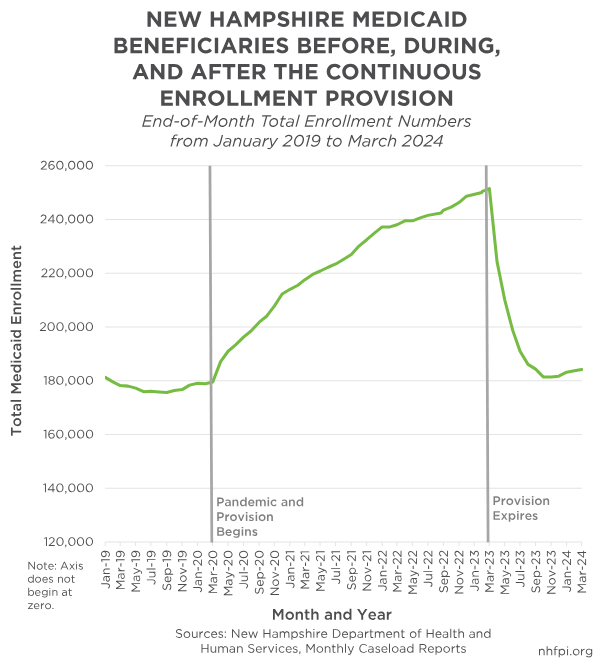
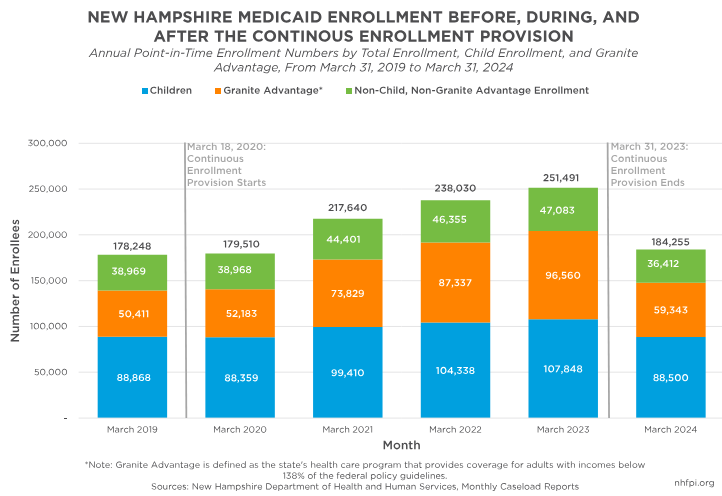
Total Medicaid enrollment numbers have drastically declined since the beginning of the unwind, with the sharpest declines occurring between March and May of 2023. According to monthly DHHS caseload data, total enrollment stood at 251,491 individuals on March 31, 2023, shortly before the unwind went into effect. Exactly one year later, as of March 31, 2024, the total has dropped by 26.7 percent, with 184,255 current enrollees. Despite this sharp decline, total Medicaid enrollment numbers remain higher than they were before the PHE, with 178,248 total enrollees at the end of March 2019 and 179,510 total enrollees at the end of March 2020, when the continuous enrollment provision first took effect.
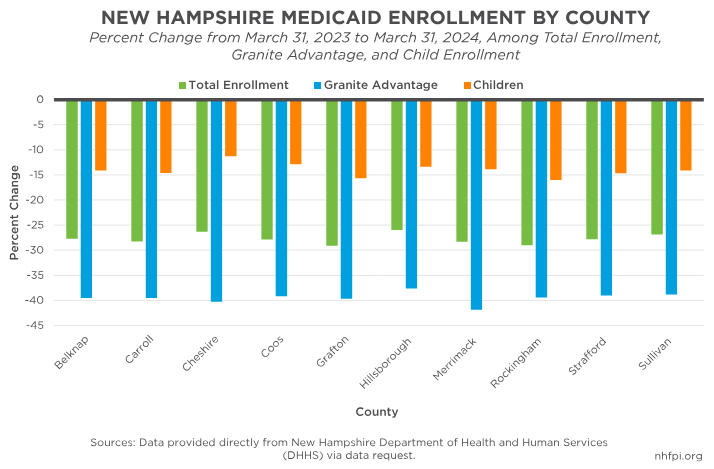
County-specific Medicaid enrollment has followed enrollment trends similar to those seen across the state. According to data provided by the DHHS, total Medicaid enrollment gradually declined from 2016 to 2020, before substantially increasing from 2020 to 2023 during the COVID-19 pandemic and the continuous enrollment provision. Between March 2023 and March 2024, enrollment decreases were similar across all counties, with slightly larger percentage decreases seen across Grafton (-29.13 percent) and Rockingham (-29.06 percent) Counties. During this same period, children enrolled in Medicaid faced smaller percent changes, with slightly larger decreases seen again in Grafton (-15.71 percent) and Rockingham (-15.99 percent) Counties. County-specific data for Granite Advantage enrollees shows substantially larger percentage decreases when compared to other groups, which is similar to statewide enrollment trends from March 2023 to March 2024. While numbers have generally been similar across counties, March 2024 enrollment percentages could change slightly if new enrollees retroactively gain coverage in the future.
Medicaid enrollees have the voluntary option to self-identify their race among categories offered on their Medicaid applications. Granite Staters identifying as American Indian or Alaska Native, white, and Asian experienced the largest percent decreases in Medicaid enrollment from March 2023 to March 2024, with decreases of 33.6 percent, 28.9 percent, and 27.5 percent, respectively. Those identifying as Black (-26.0 percent), Native Hawaiian or Pacific Islander (-25.7 percent), bi-racial/multi-racial (-21.4 percent), or another race not provided as a specific option on the application (-24.5 percent) also experienced large percent decreases. Data surrounding ethnicity was unavailable for this time period due to a lack of enrollees identifying whether they were Hispanic or non-Hispanic; enrollees can identify their race and ethnicity separately, and Hispanic ethnicity can coincide with any racial group. Due to the voluntary nature of these reported data, percentages may also reflect changes in the number of enrollees choosing to self-identify; 15.9 percent did not report their race in March 2023, and 17.1 percent did not report in March 2024.
Enrollment Changes Among Granite State Children, Granite Advantage Beneficiaries, and Individuals Experiencing Disabilities
Changes in child Medicaid enrollment have followed similar patterns to general enrollment numbers. Total enrollment among children in New Hampshire was 88,868 in March 2019. After decreasing to 88,359 enrollees in March 2020, child enrollment in Medicaid rose slowly during the pandemic to 107,848 in March 2023, just before the unwind. A year later, as of March 2024, there were 88,500 children enrolled in Medicaid, indicating an approximate reduction of 18 percent. Following procedural and policy changes resulting from CMS’s updated guidance released in December 2023, child enrollment in New Hampshire has steadily increased, from 86,522 enrollees in November 2023 to 88,500 enrollees in March 2024; despite this increase, child enrollment remains lower than March 2019 levels.
Granite Advantage beneficiaries have faced the sharpest enrollment declines since the start of the unwind period. In March 2019, a year before the start of the continuous enrollment provision, there were 50,411 New Hampshire adults enrolled in the Granite Advantage program. In March 2023, just before the unwind began, there were 96,560 enrollees, which was almost double the March 2019 count. By March 2024, the total number had fallen to 59,343, which was a larger percent decrease (-38.5 percent) in enrollment relative to March 2023 than the declines for both children (-17.9 percent), and the combined count of children and adults under 65 experiencing disabilities (-17.1 percent). Similar to increases among child enrollment over the past several months, Granite Advantage enrollment rose from 57,517 in October 2023 to 96,560 in March 2024.
The number of individuals experiencing disabilities enrolled in Medicaid has also declined, resuming a trend from before the COVID-19 pandemic. According to the DHHS, total enrollment for adults and children experiencing disabilities was 17,896 on March 31, 2020 and, after rising during the pandemic, fell to 15,926 as of March 31 2024. Older adults experiencing disabilities faced similar changes, with a total of 9,282 enrollees on March 31, 2020, compared to 9,164 enrollees on March 31, 2024. Despite increases in child and Granite Advantage enrollment from November 2023 to March 2024, enrollment numbers among individuals experiencing disabilities has remained similar and continues to fall below pre-2020 figures.
Looking Ahead
The conclusion of the continuous enrollment provision has produced significant reductions in Medicaid participation across the state. Despite these sharp declines, total enrollment remains higher than before the PHE, suggesting that this multi-year eligibility and the strategies deployed to avoid unnecessary disenrollments of eligible people has helped to retain more beneficiaries. In addition, with total Medicaid enrollment rising since October 2023, Granite Staters may continue to face rising needs following the pandemic and benefit from other recent expansions to Medicaid eligibility in New Hampshire.
In April 2024, CMS issued new rules for Medicaid operations, as well as rules for helping individuals enroll in and retain Medicaid coverage. State adoption of strategies contained within these new rules may help prevent unnecessary disenrollment of eligible beneficiaries, including after the completion of unwind-related redeterminations. Targeted outreach to households with children, individuals experiencing disabilities, and Granite Advantage beneficiaries may be particularly helpful to avoid unnecessary disenrollments in the future. If they continue to be deployed, strategies learned during the unwind and policy changes designed to expand coverage may help more Granite Staters avoid losing access to health care, despite being eligible for Medicaid, in the future.
– Jessica Williams, Policy Analyst