Medicaid, a program funded jointly by the federal and state governments, helps eliminate or defray the costs of health coverage for certain populations with incomes below certain levels. The cost of providing health care coverage to Medicaid recipients varies dramatically across different groups of recipients. Children, for example, tend to be relatively inexpensive to cover. In State fiscal year 2016, low-income children made up about 64 percent of the participants in New Hampshire’s Medicaid managed care health coverage services, but only accounted for 20 percent of the costs, according to the State’s Department of Health and Human Services (DHHS).
Certain higher costs come from the enrollees who have greater needs, particularly the elderly and those with disabilities. In New Hampshire, adults with disabilities comprised 14 percent of managed care participants in State fiscal year 2016, but 41 percent of the costs. The elderly, including elderly participants with disabilities, accounted for 6 percent of enrollees and 23 percent of costs.
These percentage breakdowns for managed care services do not account for all Medicaid payments made in New Hampshire. Medicaid was a $2 billion program in New Hampshire during State fiscal year 2016. The DHHS identified managed care costs as 41 percent of service costs in Medicaid, while waiver services, including waivers for those with developmental disabilities and certain elderly individuals, accounted for about 27 percent of Medicaid costs, and payments for nursing home patients were 18 percent of the total. New Hampshire does not deviate substantially from the nation as a whole; research from the Kaiser Family Foundation indicated that, in federal fiscal year 2014, enrollees with disabilities accounted for 40 percent of Medicaid spending, while elderly enrollees were 21 percent.
Not only are long-term care services an important component of Medicaid, but Medicaid is key for the existing provision of long-term care services. The Kaiser Family Foundation estimated two of every five people with disabilities and three in five nursing home residents in New Hampshire are covered by Medicaid; Medicaid often covers services both in nursing homes and for seniors generally that are not covered by Medicare. Nationwide, the Center on Budget and Policy Priorities estimated Medicaid covers more than 60 percent of all nursing home residents and 40 percent of costs for long-term care services and supports.
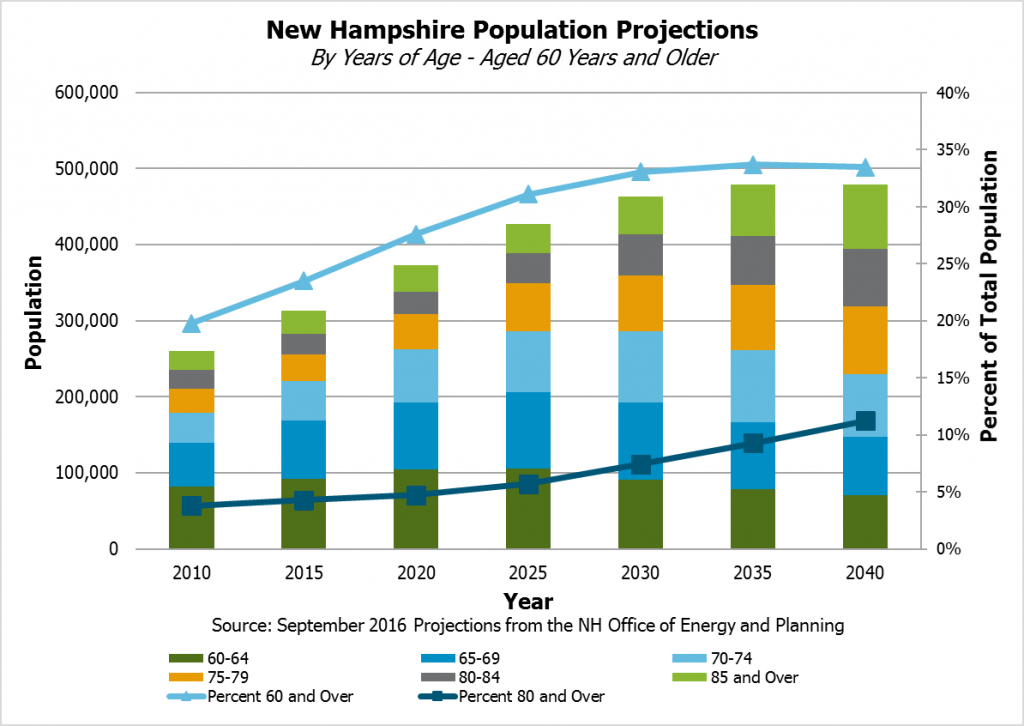
These services, especially for the elderly, are likely to be in higher demand in future years. State population projections from September 2016 indicated New Hampshire’s population aged over 85 years would increase by 60,360 people between 2010 and 2040, and the population of people 60 years or older would increase by 219,136 people. As a percentage of the population, about a third would be aged 60 or over by 2030 in these projections, up from under 20 percent in 2010, and the percentage that would be 80 years or older would rise to over 11 percent in 2040 from less than 4 percent in 2010.
Policymakers planning for Medicaid’s financial future should be cognizant of the potential for increased needs, the effects of possible policy changes on the people served, and the options available for funding these services in the long term.