One of New Hampshire’s largest government services, Medicaid helps approximately one out of every seven Granite Staters access health care. The Medicaid program is a joint federal-state partnership to eliminate or defray the costs of health coverage for certain populations with incomes below certain levels, including children, parents, pregnant women, people with disabilities, seniors and nursing home residents, and other individuals with low incomes.
People Served by Medicaid
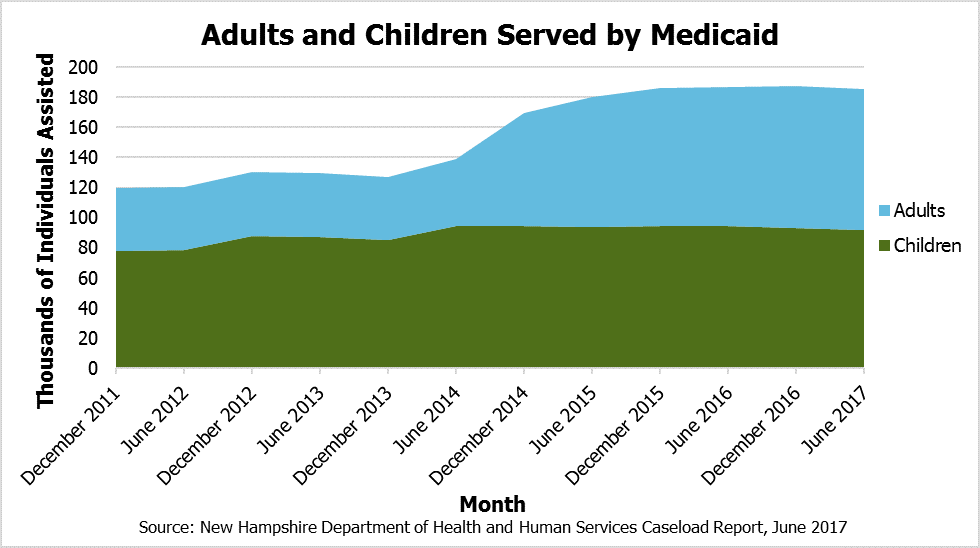
Medicaid does not provide services directly, but pays or helps to pay for health care services for more than 185,000 Granite Staters, or about 13.9 percent of the state population, based on June 2017 data from the State’s Department of Health and Human Services (DHHS). This total is approximately as many people as live in Manchester, Concord, and Dover combined. The New Hampshire Health Protection Program (NHHPP), the State’s version of expanded Medicaid under the federal Affordable Care Act, provided assistance to over 52,300 low income adults, most of whom were assisted by paying private health insurance premiums. More people are enrolled in the NHHPP than live in Coos, Sullivan, or Carroll counties.
The primary delivery system for access to short-term health services through Medicaid comes through State contracts with managed care organizations, which are private entities that manage Medicaid payments for health services in the state. The DHHS reported in May 2017 that Medicaid served approximately 133,200 individuals through Medicaid’s managed care services, including approximately:
- 90,000 children
- 20,000 people living with disabilities
- 11,300 adults with low incomes
- 8,600 senior citizens
- 2,100 pregnant women
Research from the University of New Hampshire (UNH) found that over one in four children in New Hampshire were covered by Medicaid in 2015.
Additionally, the DHHS reported roughly 10,000 people participate in the traditional “fee-for-service” Medicaid, or outside of the managed care organizations, through four Medicaid Home and Community Based Care waivers granted by the federal government for long-term care services, including for those individuals with developmental disabilities.
The Kaiser Family Foundation indicates approximately three out of every five nursing home residents in New Hampshire are covered by Medicaid.
The New Hampshire Health Protection Program
Beyond the traditional and managed care Medicaid services, DHHS snapshot data presented in May 2017 suggest the approximately 52,300 adults receiving assistance through the NHHPP tend to disenroll because of incomes rising too high to qualify; a recently analyzed two-year period also found 71 percent of recipients were not continuously enrolled over that time. Historical data analysis from the Congressional Budget Office also suggests a relatively high churn in the composition of people signed up for expanded Medicaid nationally. UNH researchers found that almost half of NHHPP enrollees receiving assistance for paying for premiums were 34 years old or younger.
The DHHS notes 3,965 unique individuals received substance use disorder services in the third quarter of 2016 through the NHHPP, and the number of individuals has risen dramatically since the NHHPP’s inception. National research from the Urban Institute suggests that states with expanded Medicaid have helped provide substantially more of certain effective types of opioid-related prescription treatments.
Paying for Medicaid
The federal government currently provides matching dollars to states to pay for the Medicaid program. For every one dollar New Hampshire contributes to pay for services eligible under Medicaid, the federal government provides at least an additional one dollar to match New Hampshire’s contribution. This “50-50 match” is the base matching rate for New Hampshire, but subsets of Medicaid have higher reimbursement rates. The NHHPP has a “95-5 match” in 2017, with the State only supplying five percent of the cost.
In total, funds from federal and State sources accounted for about $2.0 billion, or 29 percent of all State expenditures, in State fiscal year 2016, suggesting significant changes to the federal reimbursement levels would have a major impact on New Hampshire’s finances. The NHHPP alone brought $406.3 million in federal grants to New Hampshire during State fiscal year 2016.
Analysis conducted by the Center on Budget and Policy Priorities found that, between 1987 and 2015, Medicaid costs per enrollee grew at an average of 4.1 percent annually, while private insurance costs grew by an average of 6.9 percent annually. This relatively low rate of cost growth prevailed despite Medicaid functioning, in certain ways, as a high-risk pool and providing coverage comparable to private insurance by some metrics.
The Future of Medicaid
Changes to Medicaid’s funding structure have been debated at the national level within Congress’s discussions of overhauling federal health care policy. A variety of proposed changes would likely reduce federal grants to New Hampshire, with the State estimating a recent proposal would reduce grants by $1.4 billion in the first decade. Depending on the manner in which New Hampshire policymakers respond, a funding change of that magnitude could mean profound modifications to both who receives assistance through Medicaid and how much assistance is provided.
New Hampshire faces potential challenges beyond the potential for federal changes. An aging population raises the prospects of higher average health care costs per individual and potentially higher caseloads. In addition, the NHHPP’s authorization is set to expire on December 31, 2018. New Hampshire legislators will have to make changes to State law between now and the end of 2018 if they desire to maintain coverage for NHHPP enrollees and continue to receive federal grants at the enhanced match rate.