Summary and Key Highlights
Older adults and adults with physical disabilities, including those who have trouble performing day-to-day tasks, may require long-term services and supports, which can be provided through professional health and personal care providers. For adults who are financially eligible, Medicaid can cover the cost for long-term supports and services. In New Hampshire, these services are provided primarily in two settings: nursing facilities and in home or community-based settings.
Nursing facilities provide 24-hour care to their residents in an institutional setting. In New Hampshire, Medicaid funded an average of 3,624 enrollees in nursing facility beds monthly in State Fiscal Year 2021. Home and community-based care providers deliver services to people in their homes, in assisted living facilities, or in other settings. These Medicaid services for older adults and adults with physical disabilities are funded through the Choices for Independence Medicaid waiver program. Medicaid home and community-based services for people with developmental disabilities or adults with acquired brain disorders are funded through separate programs. In State Fiscal Year 2021, the average number of older adults and adults with physical disabilities enrolled in Choices for Independence each month and benefitting from home and community-based services totaled 3,795 people.
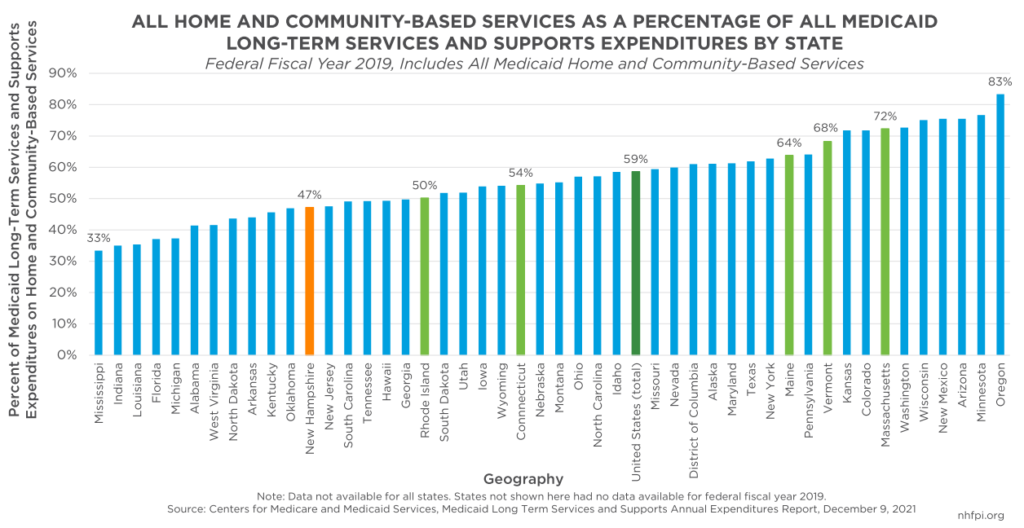
Medicaid is the largest provider of funding for long-term services and supports nationally, working to help ensure eligible people, particularly those with low incomes and limited resources, have access to needed health services. Medicaid funded 42.9 percent of all formal long-term services and supports in 2019. Home and community-based services were a key part of those expenditures. In Federal Fiscal Year 2019, home and community-based services were 58.6 percent of Medicaid long-term services and supports expenditures, including services for older adults, adults with physical disabilities, and people with developmental disabilities, and certain other populations. The other expenditures were for services delivered in institutional settings, such as nursing homes. In New Hampshire, Medicaid home and community-based services were a smaller portion of all Medicaid long-term services and supports expenditures than nationally, totaling 47.2 percent, which was also lower than all other New England states.
Medicaid services provided by nursing facilities and through the Choices for Independence program are funded by a combination of federal, State, and county revenue. The federal government pays for the largest share of total Medicaid spending in New Hampshire, and the State government pays for most of the rest of health care for Medicaid enrollees in most parts of the program. However, New Hampshire counties are required to pay for a significant portion of the costs of long-term services and supports for their residents in nursing facilities or enrolled in Choices for Independence. Nursing facilities, including nursing facilities operated by the counties, also pay the State additional funds through mechanisms called the Nursing Facility Quality Assessment and, for county nursing facilities, through a program typically called ProShare. These funds are then used to draw more federal funds through the Medicaid program, which are then disbursed back to nursing facilities through the Medicaid Quality Incentive Program and two types of ProShare payments.
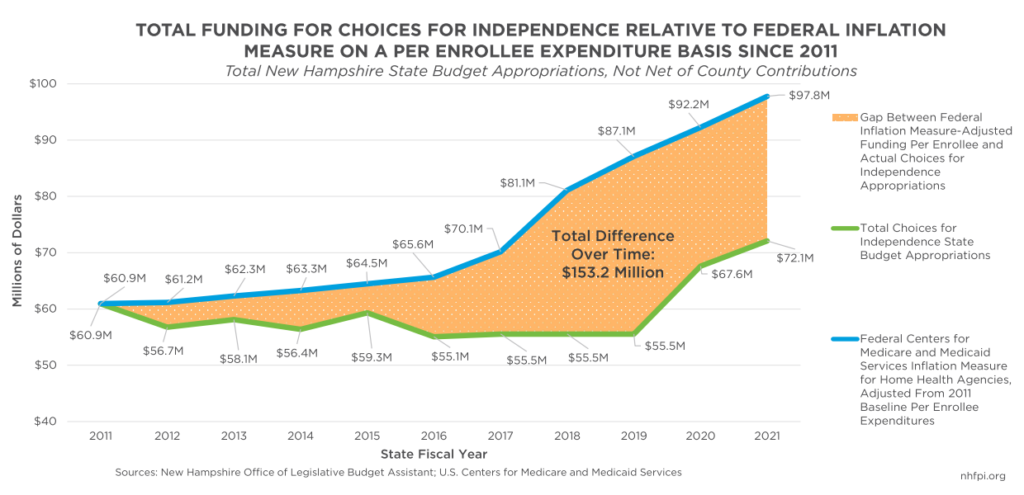
Within the requirements of the Medicaid program, the State sets reimbursement rates. These rates determine the amount of money paid to the organizations providing Medicaid services. These reimbursements are funded through the New Hampshire State Budget. In the case of nursing facilities, the State collects complex cost reporting data to set reimbursement rates, and provides funding to nursing facilities based primarily on the number of people living at a nursing facility and their health status. The funding levels for the Choices for Independence program, however, are not informed by a similar complex cost reporting structure. The amount of money in the State Budget to support people enrolled in Medicaid in nursing facilities appears to have better kept pace with the growth in costs over the last decade than funding for the Choices of Independence program. Adjusting for a key measure of inflation and for the number of program enrollees suggests that, from State Fiscal Years 2011 to 2021, State Budgets have included a total of $153.2 million fewer dollars directed to Choices for Independence services than the amount that would have kept funding for services at the same relative level. Commonly used reimbursement rates for specific Choices for Independence services also fell behind several measures of inflation for most of the last decade.
Home and community-based services are typically less expensive than nursing facilities for each enrollee funded. While individuals may receive different care in different settings, to be eligible for the Choices for Independence program, a person must be clinically eligible for a nursing home level of care. In State Fiscal Year 2021, State Budget funding appropriated for each actual Choices for Independence enrollee totaled $18,997, while for nursing facilities, funding from all sources per actual enrollee was $98,111.
State Budget funding for long-term supports and services, including both nursing facilities and home and community-based services, will become more important in New Hampshire, especially in the next two decades. More than 200,000 adults were estimated to be between age 55 and 64 years in 2019, the largest group of any other ten-year age demographic in the state. Survey data from New Hampshire indicate that more than one in five adults aged 65 to 74 years experience a disability, and more than two in five people who are age 75 years or older do as well. Providing effective services to Granite Staters, particularly including people who are more likely to need long-term services and supports, will be important for the well-being of all New Hampshire residents.
However, these services can currently be difficult to access, primarily because providers cannot find enough workers to provide all the services needed. The demographic group reaching traditional retirement age and other ongoing impacts from the pandemic have led to the size of New Hampshire’s labor force declining relative to 2019. As prices and wages quickly change with inflation accelerating, nursing facilities and home and community-based services agencies that depend on fixed Medicaid reimbursement rates for paying their staff’s wages report struggling to attract and retain workers. Recent wage data for home health and personal care aides in New Hampshire show hourly pay in the Granite State for low-wage workers is less than it is in neighboring states for the same work, which could make keeping workers in New Hampshire, or working in home and community-based services, more difficult.
Granite Staters may also have trouble accessing services due to application processes. Financial eligibility for Medicaid can be very complex. Individuals seeking to access services, either directly for themselves or people they were assisting, reported long waits for documentation and approval, and difficulty finding the right information or methods for applying for Medicaid. State data showed the median processing time for Medicaid application approval in October 2021 was 36 days for nursing facilities and 45 days for Choices for Independence waiver services. Some earlier applications reviewed by State researchers took longer than 90 days to process. These long delays mean people may not receive critically needed services.
Ongoing investments in nursing facility services and increased investments in Choices for Independence home- and community-based services, as well as the workforce that powers both industries, will be key for supporting New Hampshire’s aging population in the coming years and decades. New Hampshire has an opportunity to assess existing long-term services and supports and make thoughtful, coordinated policy decisions to help ensure investments in this essential infrastructure make progress toward a vision for improved care. Making foundational, cost-effective investments in the near-term will help create a more efficient, organized, and robust system to serve Granite Staters in need of long-term services and supports.
Policy Recommendations:
- Use flexible federal funds provided through the American Rescue Plan Act to hire public benefit navigators to help people applying for Medicaid services.
- Consider additional, systemic help for people accessing services beyond the existing frameworks for long-term services and supports in New Hampshire.
- Support home care providers with a form of payment, or commitment of future payment, prior to the formal establishment of Medicaid eligibility, or implement a form of presumptive eligibility.
- Reduce wait times for providing certain services by designating approved service providers with a pre-approved range of costs for service provision.
- Consider updates to the NH Easy system for applying for services and provide additional trainings for professionals who frequently assist people applying for services.
- Establish a centralized information portal or dashboard for providers, case managers, and navigators to quickly understand which services are available to help connect people to services faster.
- Consider a long-term program to provide a stipend or other additional funding for workforce supports to Medicaid providers, potentially funded with flexible federal funds that can be used through the end of 2026.
- Include flexibility in public wage enhancement programs for Medicaid providers to reflect related costs.
- Establish a set and more sophisticated methodology for estimating CFI waiver service delivery costs that will help inform decisions regarding reimbursement rates and help to better align future investment levels with cost changes.
- Use flexible federal funds and other resources to establish and support initiatives to grow and develop the workforce for nursing facilities and home and community-based services.
To read the full report, Long-Term Services and Supports in New Hampshire: A Review of the State’s Medicaid Funding for Older Adults and Adults with Physical Disabilities, download the PDF.
This report and its conclusions are based on independent research and analysis conducted by NHFPI, including analyses of state and national data and interviews with experts and participants in New Hampshire’s long-term services and supports systems. The full report includes citations and references to data sources, earlier research, and other publications. This research was supported by the Point32Health Foundation.