New Hampshire Choices for Independence (CFI) Medicaid Waiver services provide home- and community-based services to individuals who are chronically ill or have a disability and prefer to stay in their homes or communities but might otherwise need the level of care only provided in nursing homes, which typically result in more expensive treatment. Those in need of home- and community-based services, however, may not receive them due to a lack of available workers to deliver services. Recent data suggests that increases to Medicaid reimbursement rates, which affect the amount of resources providers have available to pay direct service care workers, may contribute to sustaining and expanding this vital workforce.
Medicaid Reimbursement Rates Have Not Kept Pace with Inflation
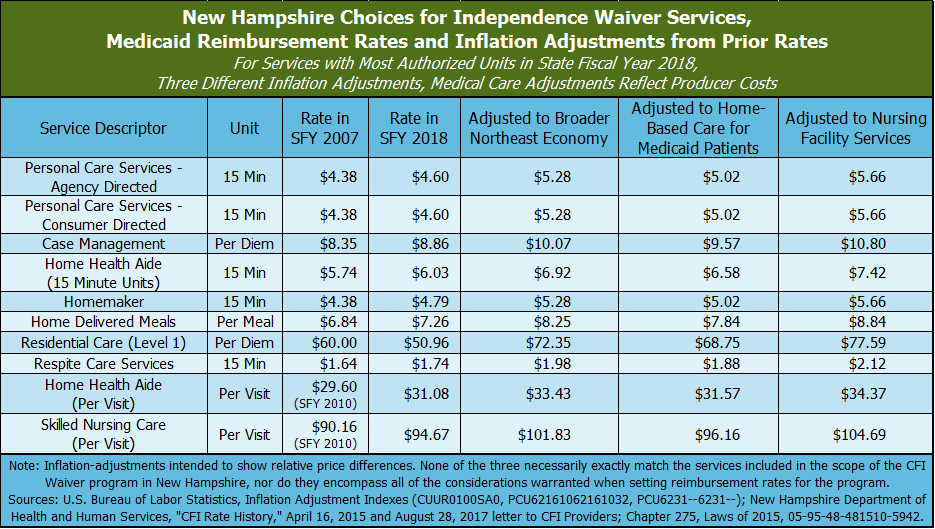
Agencies providing Medicaid services seek authorization to deliver those services from Medicaid, and then are reimbursed with federal, state, and, in some cases, county dollars for providing those services. Those reimbursements must be adjusted to match the cost of delivering services. Reimbursement rates are set by state policymakers. Key reimbursement rates for CFI Medicaid Waiver services are below their State Fiscal Year (SFY) 2007 amounts when adjusted for inflation. The SFY 2007 amounts do not necessarily reflect the true cost of providing these services, and the decline in real value suggests that agencies providing these Medicaid services are more limited in their overall ability to pay competitive wages than they were in previous years.
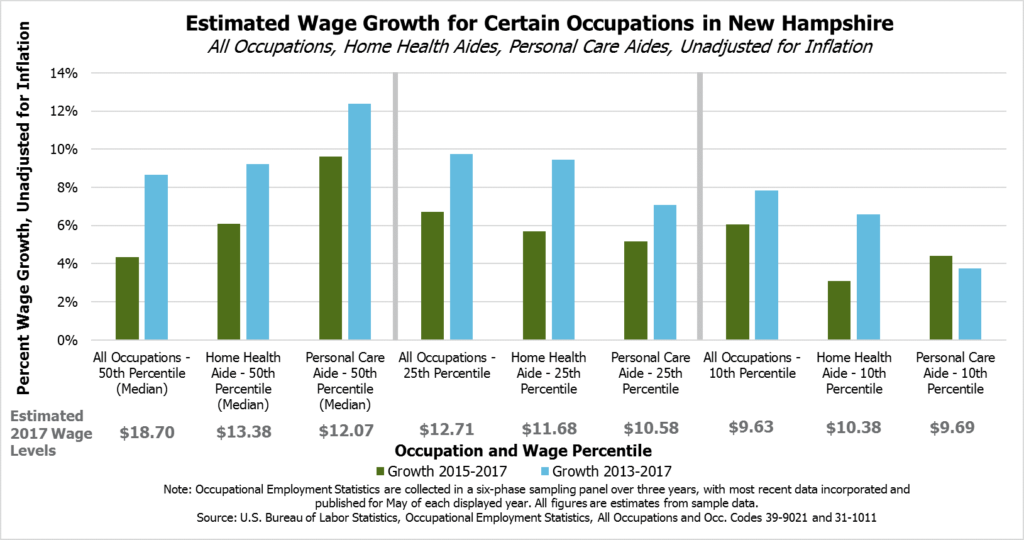
Low-Wage Home Health and Personal Care Aides See Lower Wage Growth
Home health and personal care aides making relatively low wages (at the 10th and 25th percentiles, meaning only 10 percent or 25 percent of wages offered for those occupations are lower, respectively) have seen generally lower rates of wage growth than other workers making relatively low wages in New Hampshire in recent years. While the reasons for limited wage growth are likely complex, home health care and personal care aide workers with lower wages may be more likely to have their pay affected by Medicaid reimbursement rates than those with median wages or workers in other occupations. With wages growing faster for low-wage workers throughout the economy, provider agencies relying on Medicaid reimbursements are at a competitive disadvantage.
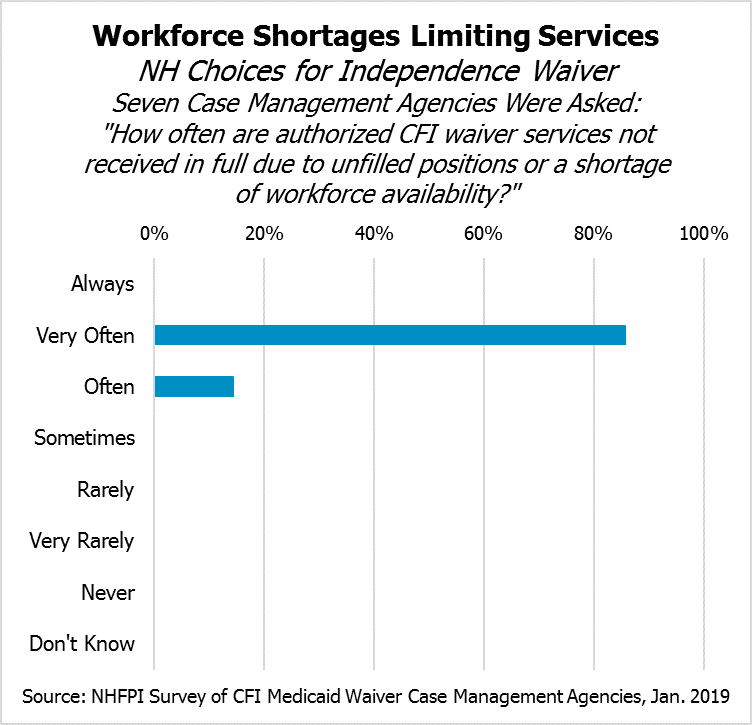
Approved CFI Services Undelivered Due to Worker Shortages
In response to a survey of New Hampshire’s seven CFI Medicaid Waiver case management agencies, all seven agencies indicated individuals may not receive CFI Medicaid Waiver services because there are not enough available workers to meet the needs. The case management agencies unanimously indicated that the availability of workers to meet CFI Medicaid Waiver service delivery needs had “Decreased Significantly” in the last three years.
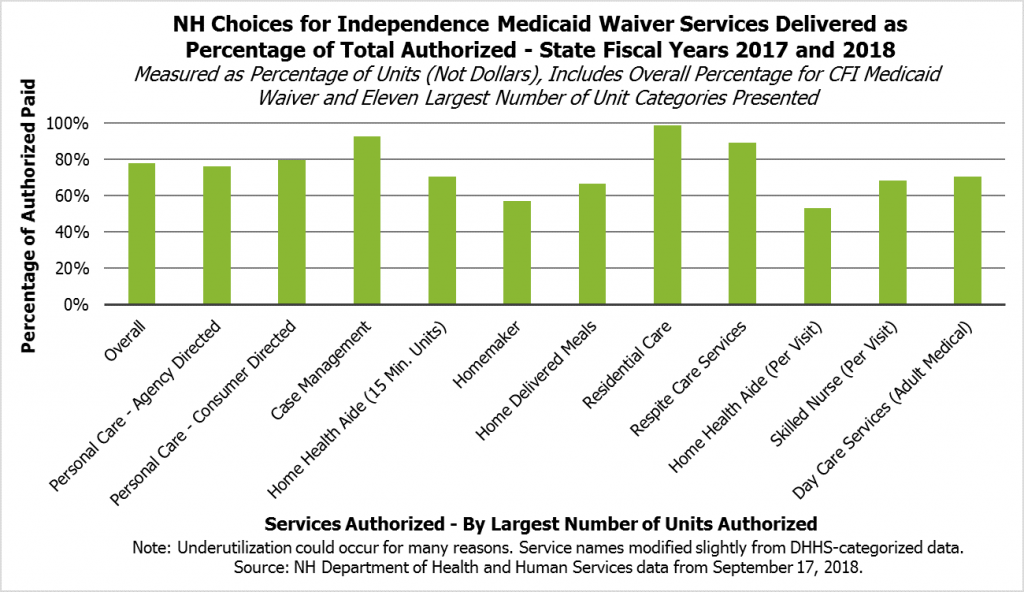
About 78 percent of the CFI Medicaid Waiver services authorized in SFYs 2017 and 2018 were paid, suggesting that some Medicaid services were not delivered. While there are likely many reasons for this gap, a lack of available workers appears to be a major factor.
For more information and analysis, see NHFPI’s Issue Brief: Medicaid Home- and Community-Based Care Service Delivery Limited by Workforce Challenges.