Thousands of New Hampshire Medicaid enrollees face potential disenrollment when the federal public health emergency declaration (PHE) associated with the COVID-19 pandemic ends. Since the PHE began on January 31, 2020, at least 59,900 more Granite Staters have become eligible for the State’s Medicaid program, increasing enrollment by 33.4 percent. However, the New Hampshire Department of Health and Human Services (DHHS) and the University of New Hampshire’s Institute for Health Policy and Practice estimate 90,800 Granite Staters may be at risk of losing coverage at the conclusion of the PHE. To help Medicaid enrollees maintain their coverage or find alternative health insurance options, New Hampshire could invest in public health navigators, trained individuals to guide Medicaid beneficiaries through the enrollment process.
Impact of the Public Health Emergency
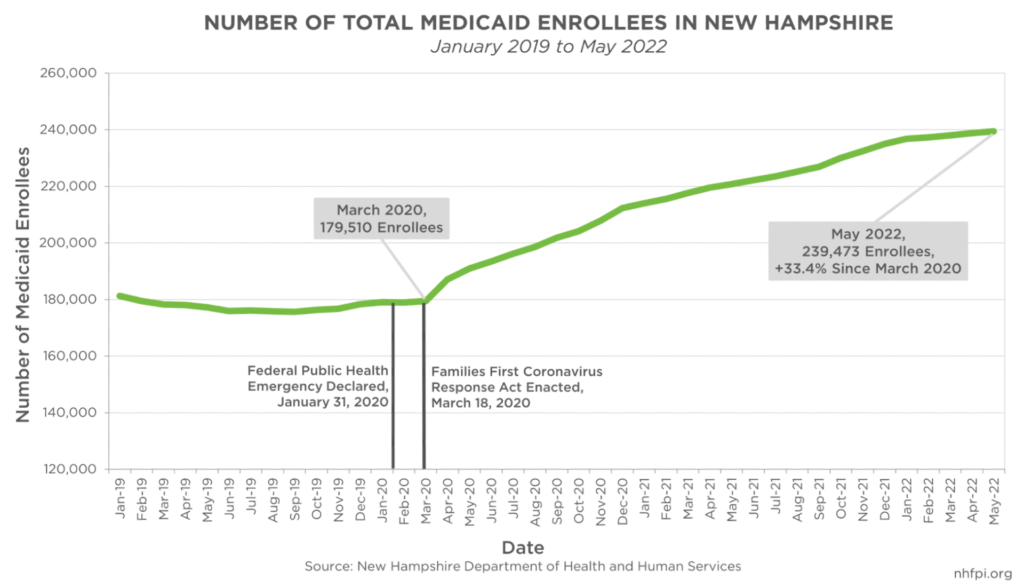
Medicaid is a partnership between the federal government and individual states to provide health coverage to families and individuals with low incomes. Medicaid beneficiaries in New Hampshire typically reside in households with incomes at or near the poverty level, with limited assets, and that include children, older adults, foster children, pregnant and post-partum women, and people with disabilities. At the end of May 2022, there were 239,473 Granite Staters enrolled in Medicaid. Of that population, 99,193 (41.4 percent) were children, which was more than the 2020 population of Nashua, the state’s second-largest city. During the same period, 10,518 Medicaid enrollees (4.3 percent) were aged 65 years or older, while 2,433 (1.0 percent) were pregnant women with low incomes, and 18,104 enrollees (7.5 percent) were adults with disabilities.
On January 31, 2020, the U.S. Secretary of Health and Human Services issued a Determination that a Public Health Emergency Exists as a result of confirmed cases of COVID-19 in the country. Since this initial Determination, the PHE has been renewed in 90-day increments, with the most recent approved on April 12, 2022. Given prior federal communications to states, the PHE will likely be extended through at least October 2022, and perhaps longer.
The PHE provided a benchmark for Congress to define a period during which the pandemic-related policies should be in effect, including regarding the potential need for higher levels of Medicaid funding and coverage. The Families First Coronavirus Response Act (FFCRA), enacted at the beginning of the COVID-19 pandemic in March of 2020, provided a 6.2 percent increase in the federal funding match rate to states, retroactive to January 1, 2020, and lasting for as long as the PHE is in effect. States accepting these additional matching funds are prohibited from disenrolling people receiving health coverage through Medicaid while the PHE is in effect.
Since the beginning of the pandemic, enrollment in Medicaid has increased. DHHS caseload reports show 59,963 more individuals accessed health services through Medicaid coverage at the end of May 2022 than did on March 31, 2020, an increase of 33.4 percent relative to the beginning of the pandemic.
Risks of Disenrollment
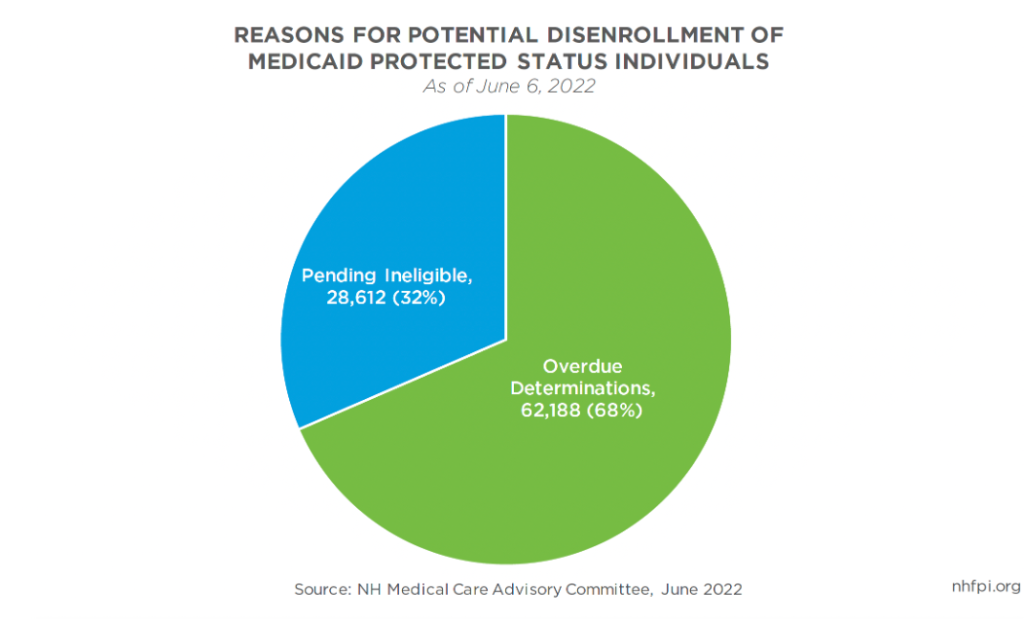
Estimates from the DHHS and the University of New Hampshire’s Institute for Health Policy and Practice show that about 90,800 Granite Staters were at risk of disenrollment at the conclusion of the PHE, as reported on June 13, 2022 by the DHHS; this total was an increase from the 87,801 reported at risk on May 9, 2022. The continuous coverage requirement of the FFCRA provides eligibility until the end of the month when the PHE concludes. After that, the DHHS will begin reviewing eligibility for enrollees, a process known as “unwinding.” Eligible enrollees could face barriers to maintaining coverage for a variety of reasons, including missing forms or notices, complex renewal and eligibility verification processes, or responses outside of required timeframes. The DHHS has worked to reach out to all beneficiaries who may be at risk of losing coverage, including by sending 75,483 pink-colored letters, which provided comprehensive information about how to maintain enrollment, as of June 6, 2022.
Of those Granite Staters that qualified for protected status during the PHE on June 6, 2022, more than two-thirds faced potential disenrollment due to overdue determinations. Thirty-two percent were identified as pending ineligible for benefits.
As of 2019, New Hampshire’s uninsured rate stood at 6.3 percent, constituting more than 84,000 uninsured Granite Staters, according to the U.S. Census Bureau. If all Granite Staters at risk of disenrollment lost coverage, the uninsured rate would more than double to about 13 percent. The Kaiser Family Foundation found that health service costs reimbursed to providers for uninsured individuals cost $33.6 billion in public dollars nationally in 2017, of which state and local governments paid $11.9 billion. Helping eligible enrollees maintain coverage would reduce the cost burden on the federal, state, and local governments.
An Opportunity for Public Benefit Navigators
Public benefit navigators could assist Granite Staters struggling with benefit enrollment. Public benefit navigators can help individuals and families apply for and access assistance for which they are eligible, reducing barriers to enrolling in public assistance programs such as Medicaid. The American Rescue Plan Act allocated nearly $1.5 billion in relatively flexible funds to the State of New Hampshire and the counties, cities, and towns within the state. The U.S. Treasury Department expressly permitted the use of these flexible federal funds to help connect people with public supports and services, including through funding public benefit navigators.
With more than 90,000 Granite Staters accessing health services through Medicaid at some risk of disenrollment without further action, the DHHS and other organizations will require time and resources to reach families that are still eligible for Medicaid or other services and effectively provide support as the PHE ends. By investing in public benefit navigators using federal funds, New Hampshire could help ensure that, regardless of when the PHE ends, Granite Staters with low incomes have access to needed health care services.
– Bobby Koolis, Policy Analyst