Earlier this week, New Hampshire state officials suspended the implementation of the work and community engagement requirements for expanded Medicaid beneficiaries until September 30. The Department of Health and Human Services (DHHS) had no information on the compliance of approximately 17,000 individuals, which would have meant up to that many individuals would have lost their health coverage starting in early August if they did not provide information and fulfill their required hours by the end of July. With this suspension, coverage losses due to noncompliance with the work requirements would not take place until early December, barring any other intervening policy changes from the state or federal governments or the pending results of legal action.
Using authority newly granted following the Governor’s signature of Senate Bill 290, the DHHS Commissioner delayed implementation of the work and community engagement requirements, citing the lack of contact with expanded Medicaid beneficiaries and the difficulty reaching individuals who might lose coverage if they were not informed about the work requirements. The DHHS indicated that, of approximately 50,000 phone calls to beneficiaries completed, less than 10 percent were answered, and only 10 percent of those who answered were able to provide necessary identifying information to discuss personal health information. Public information sessions, radio and social media advertisements, letters to beneficiaries, and 1,500 home visits were not sufficiently effective to adequately inform enrollees of the new requirements.
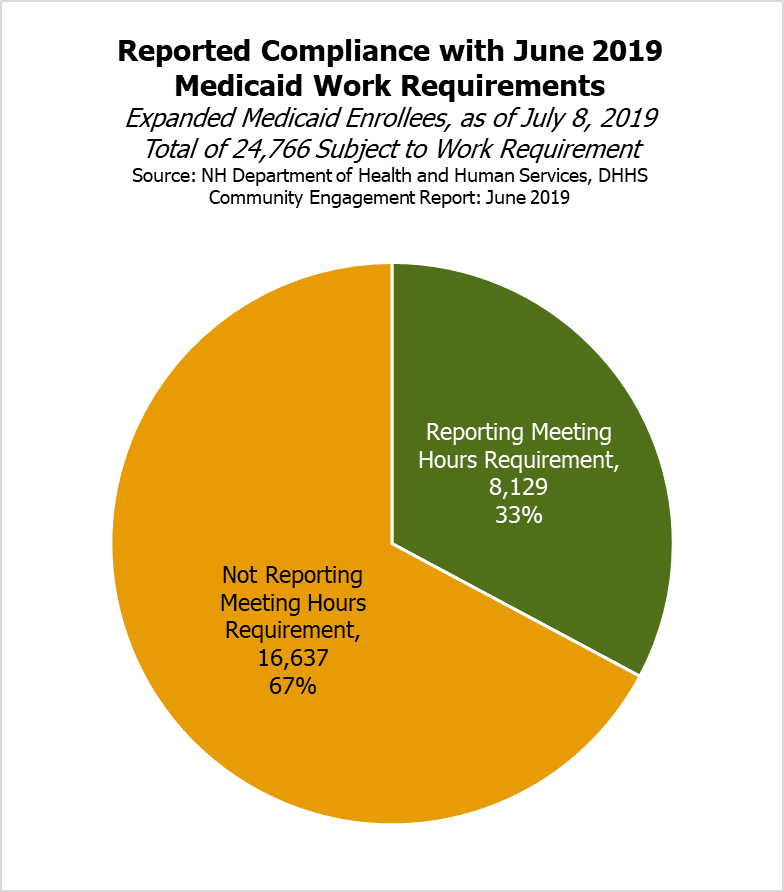
For the month of June, the State found that 24,766 beneficiaries, or about half of the enrollment population, did not have an exemption and was required to participate in the work requirement. State data as of July 8 indicated that 8,129 people, or about one-third of those required to comply, reported meeting the requirements successfully, while 16,637, or about two-thirds of those required to comply, did not do so. Senate Bill 290 required the DHHS Commissioner to suspend the work requirement if a substantial number of program members were impacted by one of a set of scenarios, including the inability of the DHHS to communicate verbally and in writing to directly counsel all members, job and transportation availability, and other “unforeseen circumstances” that are “more likely than not” to cause members to be suspended from the program. The DHHS Commissioner identified the changes made under Senate Bill 290, and the requirements to halt implementation under these circumstances, as the reasons to suspend the work requirements.
Although no future outcome is certain, coverage losses among expanded Medicaid beneficiaries subject to new work requirements appeared likely. Reported implementation challenges and confusion in New Hampshire mirrored some of the experiences in Arkansas, where 18,164 people lost health coverage. NHFPI’s May 2019 review of the potential enrollment impacts work requirements may have, based on experiences and studies in other states, suggested that implementing such requirements in New Hampshire risks causing thousands of people with limited means to lose health coverage. The data provided by the DHHS confirms that New Hampshire’s work requirement, which requires more hours of qualifying activities than Arkansas’s work requirement did, could lead to coverage losses for many Granite Staters.
Losing health coverage may lead to poorer health outcomes and reduce the likelihood that children have coverage. Evidence suggests that having health coverage reduces mortality and makes individuals more likely to access health services or to not delay treatment. Existing research also provides significant evidence that children of parents without coverage are less likely to be insured themselves.
The Governor’s signing of Senate Bill 290 made changes to the State’s work and community engagement requirements. The exemption for parents of children was expanded from those parents of children aged 5 years and under to those aged 12 years and under, and clarified that both parents or caretakers would have to be responsible for the child for one parent to be non-exempt. The changes also specifically include self-employment work as counting toward fulfilling the 100 hours of monthly work and community engagement requirements, explicitly exempt homeless individuals as defined by a certain federal statute, limit the authority of the federal Center for Medicare and Medicaid Services to alter the requirements under New Hampshire statute, and direct the DHHS to seek a federal waiver to provide 45-day retroactive coverage for enrollees found eligible, rather than no retroactive coverage under current law.
To learn more about New Hampshire’s work and community engagement requirements, see NHFPI’s May 2019 Issue Brief Medicaid Work Requirements and Coverage Losses.